Our high-quality research covers a wide spectrum within sports science and public health including the elderly, pregnant women, children and elite athletes.
Research News
-
- Top officials in sport depend on a ‘ground crew’ at homeJan. 24, 2023 6:00 AM
Doctoral candidate Hanne Sogn believes male dominance among top officials in Norwegian sport is still a problem. The hectic working day in which top officials have to be available 24/7 is one of the biggest challenges.
-
Important factors in the treatment of anterior cruciate ligament injuriesNov. 7, 2022 6:00 AM
An anterior cruciate ligament (ACL) injury is a serious knee injury that can have major consequences for knee function, activity levels and quality of life in both the short and long term. Good treatment is therefore important in order to ensure the best possible prognosis.
Our Laboratories
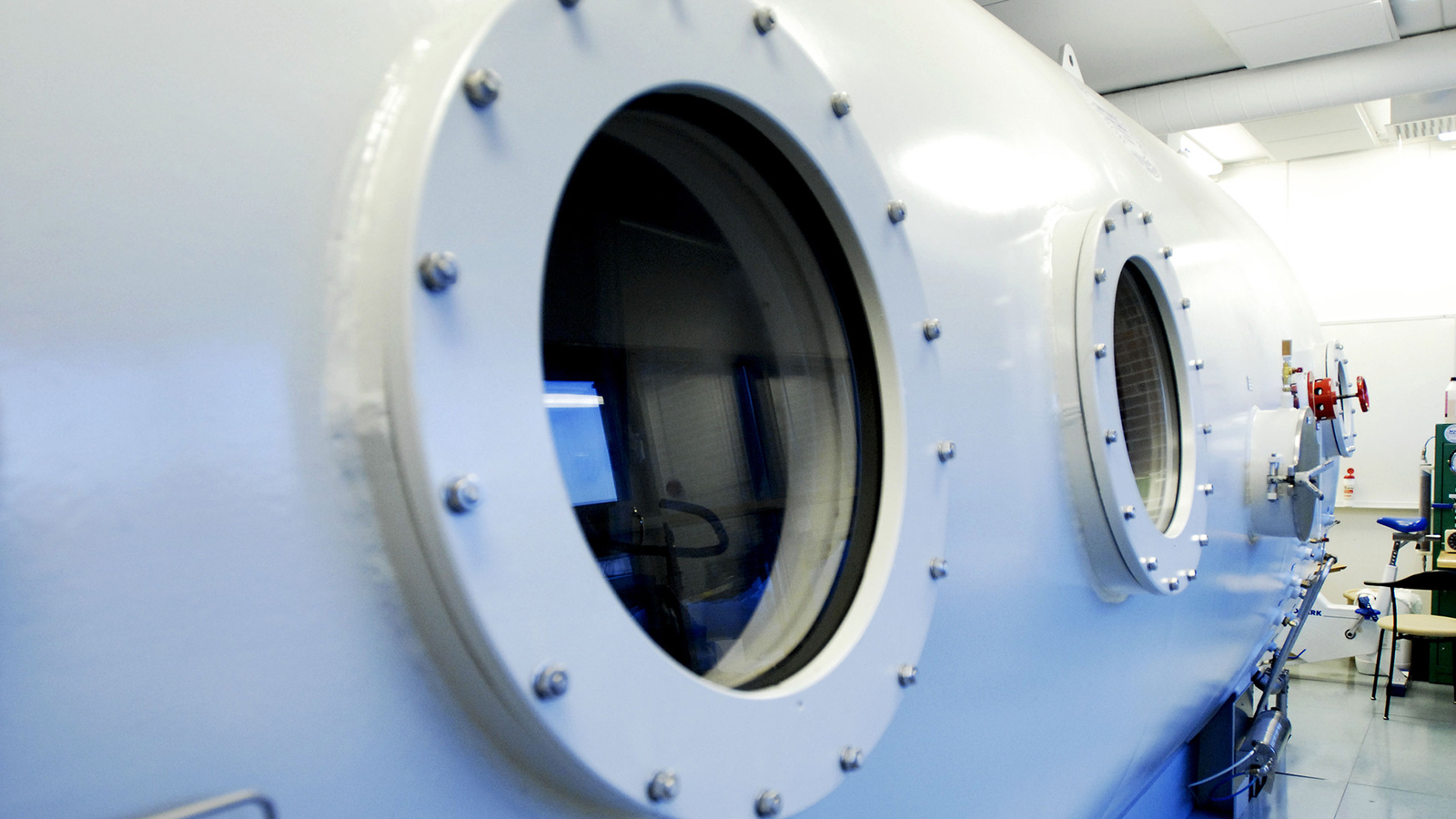
NIH has state-of-the-art laboratories and equipment for research about people in motion.
Commissioned Research

Collaborate and innovate with us. Our world-class labs stand at the ready.

International Staff
Welcome to Norway and to NIH! Our guides will help you make a smooth transition.
- Before Arrival
- After Arrival
- While in Oslo
- End of Stay
Research Centers
Forums
Survey Tools
Dissertations
NIH has a well-established doctoral program that started in 1986. See an overview of completed PhD projects.


